REGDOC-2.7.3, Radiation Protection Guidelines for Safe Handling of Decedents
Preface
This regulatory document is part of the CNSC’s radiation protection series of regulatory documents. The full list of regulatory document series is included at the end of this document and can also be found on the CNSC’s website.
Table of Contents
- 1. Introduction
- 2. Background
- 3. Guidelines for Safe Handling of Decedents
- 4. Timeframes for taking precautions
- 5. Precautions for Handling a Decedent Who Has Undergone Brachytherapy
- 6. Precautions for Handling a Decedent Who Has Undergone a Medical Procedure with an Unsealed Nuclear Substance
- 7. Handling Medical Waste
- 8. Burial and Funeral Rites
- 9. Conclusions
- 10. Contact the CNSC
- Appendix A: What is Radiation?
- Appendix B: Relevant Provincial Legislation
- Glossary
- Additional Information
1. Introduction
Radiation is commonly used in medical procedures to treat and diagnose diseases.
Some of these procedures use sources of radiation that are external to the body. The radiation passes through the patient to create an image of the body (or parts of the body), or is absorbed by the patient to treat a condition. Once the procedure is completed, no further radiation exposure is received by the patient or those around them.
For other procedures, nuclear substances are placed inside the patient’s body, either directly or by the use of implants.
When a nuclear substance is used for diagnosis, a small amount is placed directly into the body. The amount of substance decreases rapidly through radioactive decay and no further radiation exposure is received by the patient or those around them.
Some procedures involve placing a temporary implant containing a nuclear substance inside the body for a specified period of time and then it is removed. During this period, the patient is under the supervision of a physician and if they were to die, the implant would be removed before the body is released to the funeral home or crematorium. Special precautions are not necessary when handling decedents who have had a diagnostic procedure or received a temporary implant that was later removed.
This document focuses on therapeutic procedures, or treatments, that use nuclear substances. For therapeutic procedures, a larger amount of the nuclear substance is used and it may remain in the body for an extended period as it decays. This will have implications on how decedents should be handled. An overview of these procedures is provided in section 2. More information on the types of medical procedures involving nuclear substances can be found on the CNSC website.
Therapeutic procedures involving nuclear substances are generally carried out on an outpatient basis. As required by section 3 of the Radiation Protection Regulations, the treatment centre provides instructions on precautions that should be taken to minimize exposure to family members, caregivers and members of the general public. These precautions are usually needed for the first few days to a few weeks after the procedure.
If the patient dies before the nuclear substance has had a chance to decay, there may be a small amount of exposure to death-care professionals and others in the course of their work. There are precautions that can be taken to minimize the risk of exposure and to keep exposures to these workers and the public as low as possible. These are described in sections 3–5 of this document.
Handling decedents containing nuclear substances is not dangerous and any exposure received will be only a small portion of the radiation dose a person normally receives over the course of a year (from naturally occurring radioactive material, for example). There are standard radiation protection principles that can be applied to keep the dose to anyone involved as low as reasonably achievable (ALARA). The principles of radiation protection are to minimize time, to maximize distance, to use shielding whenever possible and to exercise good contamination control practices to prevent inhalation and ingestion of nuclear substances. This document outlines when and how these principles can be applied to ensure that doses to death-care professionals and other members of the public are kept as low as possible.
1.1 Purpose
This document provides death-care professionals and the public with basic guidance on handling decedents who have undergone therapeutic procedures involving nuclear substances to ensure that radiation exposure is kept below limits that have been set to protect the public. Background information is provided on procedure types, the risks they present and methods for reducing the potential for exposure.
1.2 Scope
The guidance provided in this document is for information purposes only. Diagnostic nuclear medicine procedures, where the nuclear substance decays quickly, and temporary implant brachytherapy procedures, where the source is easily removed, are not within the scope of this document. This document does not apply to animals that have had a therapeutic procedure using nuclear substances.
This document provides guidance on how bodies containing radioactive implants can be safely cremated. However, Ontario, Quebec and Saskatchewan prohibit the cremation of bodies that contain radioactive implants. See appendix B for the relevant excerpts of current provincial legislation.
2. Background
2.1 Therapeutic nuclear medicine
Therapeutic nuclear medicine is the administration of nuclear substances, either orally or via injection, for therapeutic procedures, such as radioactive iodine for the treatment of thyroid cancer or hyperthyroidism. The desired therapeutic outcome in these cases is to kill the diseased cells. The bodily fluids, organs and other parts of the body may still contain radioactive material for some time after the procedure.
2.2 Manual brachytherapy (permanent implants)
Manual brachytherapy is a type of cancer treatment that uses sealed radioactive sources. These sources, commonly referred to as "seeds", are implanted into or placed close to a tumour to deliver a therapeutic dose of radiation while limiting the exposure to surrounding healthy tissues. The most common application is the treatment of prostate cancer.
The seeds are made of a titanium shell with the radioactive source enclosed. The seeds are smaller than a grain of rice (see figure 1). On average, 100 seeds are distributed throughout the affected tissue. The seeds remain within the organ indefinitely and the nuclear substance decays in the body over time.
Figure 1: Radioactive seeds

2.3 Nuclear substances
The nuclear substances involved in nuclear medicine and manual brachytherapy are commonly called radioisotopes. The quantity of the radioisotope, called the “activity”, varies by procedure. Each radioisotope also decays at a different rate. Once the material fully decays to a stable isotope, it is no longer radioactive. Table 1 provides examples of some radioisotopes and their medical applications.
Table 1: Typical applications of nuclear substances used for therapeutic procedures
| Radioisotope | Typical applications |
|---|---|
| Iodine-125 | brachytherapy, to treat prostate cancer |
| Palladium-103 | brachytherapy, to treat prostate or breast cancer |
| Strontium-89 | nuclear medicine, to provide pain relief from bone cancer |
| Yttrium-90 | nuclear medicine, to treat a variety of conditions and diseases such as arthritis and various cancers |
| Phosphorus-32 | nuclear medicine, to treat a family of diseases characterized by increased blood cell production |
| Iodine-131 | nuclear medicine, to treat various types of tumours and hyperthyroidism |
2.4 Release from treatment centre
Both nuclear medicine and brachytherapy procedures are done routinely on an outpatient basis. Before leaving the treatment centre, the patient and/or their caregiver are instructed on precautions that should be taken to limit exposure to others. These precautions are only needed for a limited period of time, after which the radioactivity of the nuclear substance will have decayed to a level that the precautions are unnecessary.
If the patient were to die, the nature of the exposure to those around the decedent during preparation of the body or the remains may be different compared to when the patient was alive. As such, special precautions may be required. These precautions are described in section 4 and 5 of this document.
2.5 Information about the procedure
When a death-care professional receives a body and becomes aware that the individual had undergone one of these procedures, the following information should be obtained from family or caregivers:
- the type of radiation procedure (e.g., therapeutic nuclear medicine or a brachytherapy implant and the nuclear substance used)
- where and when the procedure took place
- contact information for the treatment centre
The information can also be obtained by contacting the radiation safety officer at the treatment centre. This person is responsible for all matters relating to radiation safety at the treatment centre.
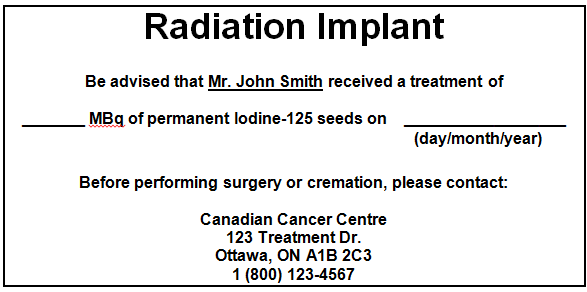
Figure 2 shows an example of a wallet card given to a patient after the procedure. The treatment centre’s radiation safety officer can provide more information if required.
Figure 2: Example of a brachytherapy implant card
3. Guidelines for Safe Handling of Decedents
This section provides general radiation protection guidelines. Sections 4 and 5 provide more specific details.
3.1 Time
The amount of radiation exposure is directly related to the time spent in close proximity to the body or the remains.
- Minimize time close to the body or remains; spend only as much time as is necessary. To reduce time, additional efforts should be made to plan and prepare for the handling of decedents in order to complete the required tasks as efficiently as possible.
3.2 Distance
The further a person is from a nuclear substance, the lower the dose will be.
- Maximize distance from the body or remains, as practicable.
- Use tools to avoid direct contact with organs or tissues that might contain the nuclear substance.
3.3 Personal protective equipment
Most safety standards already require that personal protective equipment is worn, even when no nuclear substances are involved, but it is also important for radiation safety to prevent the possibility of ingesting or inhaling a nuclear substance.
- Wear appropriate personal protective equipment, such as disposable gloves, a face mask, safety eyewear and a disposable gown while handling the body or any remains.
4. Timeframes for taking precautions
Once all the information about the procedure is acquired, a decision can be made as to whether precautions should be taken. Table 2 shows the time frames during which the CNSC recommends that precautions be taken to ensure that any doses to the workers and the general public are kept as low as reasonably achievable. No precautions are necessary if the time since the procedure is greater than the time listed in the table.
Table 2: Timeframes for taking precautions discussed in sections 5 and 6
| Nuclear substance | Autopsy | Embalmment | Cremation |
|---|---|---|---|
| Iodine-125 | 2 years | 1 month | 2 years |
| Palladium-103 | 3 months | 1 month | 3 months |
| Strontium-89 | 2 years | 2 weeks | 1 year |
| Yttrium-90 | 6 weeks | 2 weeks | 6 weeks |
| Phosphorus-32 | 5 months | 2 months | 5 months |
| Iodine-131 | 2 months | 2 months | 2 months |
If two years have passed since the procedure was performed, no precautions are necessary regardless of the substance used.
5. Precautions for Handling a Decedent Who Has Undergone Brachytherapy
5.1 Iodine-125 and palladium-103
If the person underwent a brachytherapy procedure more than two years ago, no extra precautions are needed and the body can be prepared in the usual manner. If it is less than two years since the brachytherapy procedure, follow the recommended precautions in sub-sections 5.1.1, 5.1.2 and 5.1.3. The times given below are for iodine-125 and palladium-103.
5.1.1 Autopsy and embalmment
The nuclear substance will remain sealed within the seed and will be contained within a single organ or site. There is minimal risk of the presence of contamination as long as the seeds have not ruptured. There will be a small amount of dose received while conducting the autopsy and embalmment due to external radiation from the nuclear substance within the body.
Precautions
- If the patient has died within two years of a procedure with iodine-125 or three months for palladium-103, the tissue around the implant should remain intact during the autopsy. This will provide shielding from the nuclear substance and prevent unintended dissection of the seeds. In the case of implants in the prostate, for example, the prostate should remain intact.
- Autopsies should be limited to two hours if the patient has died within one month of the procedure.
- Embalming should be limited to two hours if the patient has died within one month of the procedure.
- If it is essential to remove the prostate (for the purposes of the examination), the treatment centre’s radiation safety officer should be consulted.
5.1.2 Cremation
Precautions for death-care professionals
If the patient has died within two years of a procedure with iodine-125 or three months with palladium-103:
- Use disposable gloves, a face mask, safety eyewear and a disposable gown when cremating the body and handling the cremated remains.
- Rake out the cremation chamber as thoroughly as possible to avoid contamination of the cremated remains from future cremations.
- Leave the exhaust fan on at all times until the cremated remains are placed in their final container and the area has been cleaned.
- Avoid pulverizing the remains to prevent the contamination of equipment and rupture of any remaining seeds.
Precautions for handling cremated remains
If the patient has died within two years of a procedure with iodine-125, or within three months with palladium-103:
- Store the cremated remains in a closed container, preferably one made of stainless steel. This will shield the radiation more than some other materials.
- Store the cremated remains in an area that is not subject to high occupancy (e.g., in a room that is rarely occupied or in a basement).
- Do not scatter the cremated remains for a period of two years of a procedure with iodine-125 or three months of a procedure with palladium-103. The date on which cremated remains may be scattered should be placed on the container.
- Do not make memorial keepsake jewellery or tattoos with the cremated remains.
5.1.3 Alkaline hydrolysis
Precautions
Do not dispose of the body by alkaline hydrolysis if the patient has died within two years of a procedure with iodine-125, or within three months with palladium-103.
6. Precautions for Handling a Decedent Who Has Undergone a Medical Procedure with an Unsealed Nuclear Substance
Nuclear medicine involves the use of unsealed nuclear substances, which once in the body, can be present in tissue and bodily fluids for a period of time depending on the procedure. In some cases, handling the decedent can present a contamination hazard (e.g., through exposure to bodily fluids during an autopsy), where there is potential for the nuclear substance to be inhaled, ingested, absorbed through the skin from a puncture wound or skin contamination. Additionally, the radiation from nuclear substances may penetrate through the decedent’s body and represent an external hazard to those around it.
There are a variety of nuclear substances used for therapeutic purposes. Because of differences in the application and properties of the nuclear substances, precautions are addressed specifically according to some of the most commonly used nuclear substances, and/or those that present a special case, because of either their long decay time or the purpose of the treatment (curative versus palliative, which may impact the likelihood of death in the months following the procedure).
In all of the examples, if the person underwent a nuclear medicine procedure more than two years ago, no extra precautions are needed and the body can be prepared in the usual manner. If it has been less than two years since the nuclear medicine procedure, follow the recommended precautions in subsections 6.1 to 6.4.
6.1 Strontium-89
Strontium-89 is used to lessen bone pain associated with various cancers, particularly advanced prostate cancer that has spread to the bone. The treatment is typically administered for advanced stages of the disease and is done so for palliative purposes. As such, it is possible that the patient may die from the disease within a few months of the procedure.
6.1.1 Autopsy and embalmment
Precautions
- Wear disposable gloves, gown and face mask when handling the body to avoid the presence and spread of contamination and rinse any instruments after use if the patient has died within two weeks of the procedure.
- Wear safety glasses or goggles.
- Do not directly handle bones with lesions if the patient has died within two years of the procedure. Use tools and tongs to avoid direct contact with the bones when performing autopsies. If this is not possible, the treatment centre’s radiation safety officer should be consulted.
- During embalmment, minimize direct contact with the arterial drainage tube or use handling tools to manipulate it.
6.1.2 Cremation
Strontium-89 will concentrate in the bones and remain in the cremated remains after cremation.
Precautions for death-care professionals
If the patient has died within one year of the procedure:
- Use heavy rubber gloves, a face mask, safety eyewear and a disposable gown when cremating the body and handling the cremated remains.
- Rake out the cremation chamber as thoroughly as possible to avoid contamination of future cremations.
- Leave the exhaust fan on at all times until the cremated remains are placed thin their final container and the area has been cleaned.
- Avoid pulverizing the cremated remains to prevent the contamination of equipment.
Precautions for handling cremated remains
- Store the cremated remains in a closed container, preferably made of stainless steel. This will shield the radiation more than a material such as wood.
- Do not scatter the cremated remains for a period of one year from the date the patient was treated. The date on which cremated remains may be scattered should be placed on the container.
- Do not make memorial keepsake jewellery or tattoos with the cremated remains for a period of one year from the date the patient was treated.
- Do not directly handle/touch the cremated remains for a period of one year from the date the patient was treated
6.1.3 Alkaline hydrolysis
Precautions
Do not dispose of the body by alkaline hydrolysis for one year following the procedure.
6.2 Yttrium-90
Yttrium-90 is used to treat a variety of conditions and diseases such as arthritic conditions and various forms of cancer.
6.2.1 Autopsy and embalmment
The safety precautions below for autopsies and embalmment are designed to minimize the risk of contamination as some of the initially delivered nuclear substance will be present in body excretions, such as blood and urine for approximately one week after the procedure. The precautions are also designed to minimize doses to the skin associated with beta radiation, in cases where the body is opened and the death care worker may not be fully shielded from the external beta radiation.
Precautions
- If death has occurred within six weeks of the procedure, then the treatment centre’s radiation safety officer should be consulted.
- Use disposable gloves, gowns and masks when handling the body to avoid skin contamination and rinse any instruments after use if the patient has died within six weeks of the procedure.
- Wear safety glasses or goggles.
- During embalming, minimize direct contact with the arterial drainage tube if death has occurred within two weeks of the procedure. If this is not possible, then the treatment centre’s radiation safety officer should be consulted.
6.2.2 Cremation
Precautions for death-care professionals
If the patient has died within six weeks of the procedure:
- Use heavy rubber gloves, a face mask, safety eyewear and a disposable gown when cremating the body and handling the cremated remains.
- Rake out the cremation chamber as thoroughly as possible to avoid contamination of future cremations.
- Leave the exhaust fan should be on at all times until the cremated remains are placed in their final container and the area has been cleaned.
- Avoid pulverizing the cremated remains to prevent the contamination of equipment.
Precautions for handling cremated remains
- Store the cremated remains in a closed container, made of plastic or wood, but preferably leaded Plexiglas, if feasible.
- Do not scatter the cremated remains for a period of six weeks from the date the patient was treated. The date on which cremated remains may be scattered should be placed on the container.
- Do not make memorial keepsake jewellery or tattoos with the cremated remains for a period of six weeks from the date the patient was treated.
- Do not directly handle/touch the cremated remains for a period of six weeks from the date the patient was treated.
6.2.3 Alkaline hydrolysis
Precautions
Do not dispose of the body by alkaline hydrolysis for six weeks following the date the patient was treated.
6.3 Phosphorus-32
Phosphorus-32 is used to treat a family of diseases characterized by increased blood cell production. Due to the type and characteristics associated with its radioactive decay, the hazard associated with the radiation while the body is closed is very low.
6.3.1 Autopsy and embalmment
The following safety precautions are designed to minimize the risk of contamination, as some of the initially delivered nuclear substance will be present in body excretions such as blood and urine for approximately one week after the procedure. These precautions are also meant to minimize doses to the skin associated with beta radiation, in cases where the body is opened and the death care worker may not be fully shielded from the external beta radiation.
Precautions
- Use disposable gloves, gowns and masks when handling the body to avoid contamination and rinse any instruments after use if the patient has died within two weeks of the procedure.
- Wear safety glasses or goggles.
- During embalming, do not have direct contact with the arterial drainage tube if death has occurred within two months of the procedure. If this is not possible, then the treatment centre’s radiation safety officer should be consulted.
- If the patient has died within five months of the procedure, the treatment centre’s radiation safety officer should be consulted.
6.3.2 Cremation
Precautions for death-care professionals
If the patient has died within five months of the procedure:
- Use heavy rubber gloves, a face mask, safety eyewear and a disposable gown when cremating the body and handling the cremated remains.
- Rake out the cremation chamber as thoroughly as possible to avoid contamination of future cremations.
- Leave the exhaust fan on at all times until the cremated remains are placed in their final container and the area has been cleaned.
- Avoid pulverizing the cremated remains to prevent the contamination of equipment.
Precautions for handling cremated remains
- Store the cremated remains in a closed container, made of plastic or wood but preferably leaded Plexiglas, if feasible.
- Do not scatter the cremated remains for a period of five months from the date the patient was treated. The date on which cremated remains may be scattered should be placed on the container.
- Do not make memorial keepsake jewellery or tattoos with the cremated remains for a period of five months from the date the patient was treated.
- Do not directly handle/touch the cremated remains for a period of five months from the date the patient was treated.
6.3.3 Alkaline hydrolysis
Precautions
Do not dispose of the body by alkaline hydrolysis for a period of five months following the date the patient was treated.
6.4 Iodine-131
Iodine-131 is the most widely used of all nuclear substances in therapeutic applications. It is used to treat thyroid conditions, specifically hyperthyroidism and thyroid cancer.
6.4.1 Autopsy and embalmment
Because of the volatility of this nuclear substance and the wide variety of uses it has, generic precautions that cover all cases are not appropriate. As such, these should be managed on a case-by-case basis.
Precautions
- If the patient has died within two months of the procedure, then the treatment centre’s radiation safety officer should be consulted.
6.4.2 Cremation
Precautions for death-care professionals
- If the patient has died within two months of the procedure, then the treatment centre’s radiation safety officer should be consulted.
Precautions for handling cremated remains
- Store the cremated remains in a closed container, preferably made of stainless steel.
- Do not scatter the cremated remains for a period of two months from the date the patient was treated. The date on which cremated remains may be scattered should be placed on the container.
- Do not make memorial keepsake jewellery or tattoos with the cremated remains for a period of two months from the date the patient was treated.
- Do not directly handle/touch the cremated remains for a period of two months from the date the patient was treated.
6.4.3 Alkaline hydrolysis
Precautions
Do not dispose of the body by alkaline hydrolysis for a period of two months following the date that the patient was treated.
7. Handling Medical Waste
Any bodily fluids can be disposed of in the normal fashion. Any tissue that is removed during autopsy should be returned to the body for cremation or burial unless this is explicitly forbidden by provincial regulations.
8. Burial and Funeral Rites
Burial of bodies with residual activity can be performed at any time. Burial usually involves placing the decedent underground in a wood or metal casket. Because of the shielding from the casket and the earth, the radioactivity will pose no safety concerns. For natural burial, where the body decomposes naturally in the earth, the radioisotope will decay before it can contaminate any part of the surrounding environment.
Similarly, transportation of bodies with residual activity is not a concern. Note that the regulations governing transport of nuclear substances provide a specific exemption from the application of those regulations for nuclear substances implanted in or incorporated into a person for medical purposes. See subsection 2(b) of the Packaging and Transport of Nuclear Substances Regulations, 2015.
9. Conclusions
By following the precautions described in this document, the radiation hazards involved with handling decedents containing residual radioactivity are minimal. It is important to ensure that professionals, family members of the decedent, and the environment are protected while allowing the wishes of the decedent and their loved ones to be met, to the extent possible.
The handling of a body with residual radioactivity can be performed safely using the recommendations provided herein to reduce and avoid radiation risk.
10. Contact the CNSC
For more information, contact the CNSC at:
Phone: 1-800-668-5284 (in Canada) or 613-995-5894 (within the National Capital Region or outside Canada)
Fax: 613-995-5086
Email: cnsc.info.ccsn@cnsc-ccsn.gc.ca
Mail: Canadian Nuclear Safety Commission
280 Slater Street
P.O. Box 1046 Station B
Ottawa, ON K1P 5S9
For information in case of a death during non-business hours, please call CNSC's 24-hour duty officer at 613-995-0479 or 1-844-879-0805 (toll free in Canada and the U.S.).
Appendix A: What is radiation?
Radiation is energy transmitted in the form of waves or streams of particles. Radiation has always been present and is all around us in many forms. Life has evolved in a world filled with radiation, which is part of our everyday lives.
Radiation can be described based on the effect it has on things. There are two types of radiation: ionizing and non-ionizing. Ionizing radiation includes the radiation that comes from both natural and man-made radioactive materials such as cosmic rays, nuclear power plants, X-ray machines, and nuclear substances used in medical procedures. Non-ionizing radiation is a lower energy radiation such as radio waves, ultraviolet rays, microwaves, and sunlight.
When ionizing radiation penetrates matter, such as the human body, it deposits energy. The degree of a biological effect on the human body will depend on the amount of radiation deposited, the type of radiation and the tissue or organ in the body that has been exposed. The amount of energy deposited and its effect are represented by a quantity called a "dose". Various activities listed in the table below put doses into perspective:
| Effective dose (mSv) | Limit or activity |
|---|---|
| > 1000 | Acute dose that may cause symptoms of radiation sickness |
| 500 | Annual dose limit for persons carrying out emergency work (currently in section 15 of the Radiation Protection Regulations) |
| 150 | Average annual exposure to astronauts working on the International Space Station |
| 100 | Five-year dose limit for nuclear energy workers |
| 50 | Annual dose limit for nuclear energy workers (section 13 of the Radiation Protection Regulations) |
| 7 | Typical chest CT (computed tomography) scan |
| 1.8 | Annual Canadian average of natural background radiation |
| 1 | Annual public dose limit (section 13 of the Radiation Protection Regulations) |
| 0.1 | Typical chest X-ray |
| 0.02 | Typical cross-Canada flight |
| 0.001 | Typical dose from living one year within a few kilometres of an operating nuclear power plant in Canada |
Appendix B: Relevant Provincial Legislation
Most provinces and territories have no legislation for handling human remains that contain nuclear substances. The exceptions are Saskatchewan, Ontario and Quebec.
Note that the excerpts from the provincial legislation below reflect the current status as of writing this document. The Acts and Regulations should be consulted directly for the most current information.
Saskatchewan
Section 28 of the Funeral and Cremation Services Regulations states that "no person shall provide human remains to a crematorium for cremation if the person knows or ought reasonably to know that: a) radioactive implant is in the human remains;"
Ontario
The following provisions of the general regulations made under the Funeral, Burial and Cremation Services Act are relevant to this document:
- paragraph 31(2)(b) states that “"he crematorium operator shall not permit the cremation of a dead human body if…the body has a pacemaker or radioactive implant, is in a casket that consists of or has on or in it material made of or containing non-flammable or hazardous material or chlorinated or fibre-reinforced plastic, other than incidental metal used in the construction of the casket or accompanying material."
- paragraph 31(3) states that "The crematorium operator may contract out or arrange for the removal of a pacemaker or radioactive implant from a dead human body if the person carrying out the removal is a person described in section 52."
- paragraph 33(7) states that "The funeral establishment operator may contract out or arrange for the removal of a pacemaker or radioactive implant from a dead human body if the person carrying out the removal is a person described in section 52."
- paragraph 35(3) states that "The transfer service operator may contract out or arrange for the removal of a pacemaker or radioactive implant from a dead human body if the person carrying out the removal is a person described in section 52."
- section 52 states that "An operator shall not engage a person to remove a pacemaker or a radioactive implant from a dead human body unless,
(a) the person holds a Funeral Director – Class 1 licence and is acting on behalf of an operator that holds a Funeral Establishment Operator – Class 1 licence or a Transfer Service Operator – Class 1 licence;
or
(b) the person is a legally qualified medical practitioner."
Quebec
Section 42 of the Regulation respecting the application of the Act respecting medical laboratories, organ and tissue conservation and the disposal of human bodies of the Government of Quebec states the following: "A funeral director or embalmer who takes possession of a human body which might possibly contain radioisotopes must take all the necessary steps to protect the members of his staff who are called upon to handle the body, and he must take the necessary measures to eliminate any radioactive source. Every sealed source of radioactivity must be removed from a body before embalming or incineration thereof."
Glossary
For definitions of terms used in this document, see REGDOC 3.6, Glossary of CNSC Terminology.
REGDOC 3.6 is provided for reference and information, and includes terms and definitions used in the Nuclear Safety and Control Act, the regulations made under it, and CNSC regulatory documents and other publications.
The following term is being defined for the first time in the draft for public consultation. Following public consultation, the final versions of this definition will be submitted for inclusion in the next version of REGDOC 3.6.
- alkaline hydrolysis
- Also known as resomation, a process involving heating the body in a basic solution (water and lye) until the tissue dissolves. The bones are removed from the liquid, crushed into a powder and returned to the decedent’s family in a container similar to a cremation vessel.
Additional Information
- Institute of Physics and Engineering in Medicine, Report 106: UK Guidance on Radiation Protection Issues following Permanent Iodine-125 Seed Prostate Brachytherapy, London, 2012.
- Institute of Physics and Engineering in Medicine, Report 109: Radiation Protection in Nuclear Medicine, York, UK, 2014.
- International Atomic Energy Agency, Safety Report Series No. 63: Release of Patients After Radionuclide Therapy, Vienna, 2009.
- International Commission on Radiological Protection, ICRP Publication 94: Release of Patients after Therapy with Unsealed Radionuclides. Annals of the ICRP 34(2), Amsterdam, 2004.
- International Commission on Radiological Protection, ICRP Publication 98: Radiation Safety Aspects of Brachytherapy for Prostate Cancer using Permanently Implanted Sources, Annals of the ICRP 35(3), Amsterdam, 2005.
- Que, W. Radiation Safety Issues regarding the Cremation of the Body of an I-125 Prostate Implant Patient. Journal of Applied Clinical Medical Physics. 2(3): 174-77, Alexandria, VA, 2001.
CNSC Regulatory Document Series
Facilities and activities within the nuclear sector in Canada are regulated by the Canadian Nuclear Safety Commission (CNSC). In addition to the Nuclear Safety and Control Act and associated regulations, these facilities and activities may also be requirements to comply with other regulatory instruments such as regulatory documents or standards.
Effective April 2013, the CNSC's catalogue of existing and planned regulatory documents has been organized under three key categories and twenty-five series, as set out below. Regulatory documents produced by the CNSC fall under one of the following series:
- 1.0 Regulated facilities and activities
- Series 1.1 Reactor facilities
- 1.2 Class IB facilities
- 1.3 Uranium mines and mills
- 1.4 Class II facilities
- 1.5 Certification of prescribed equipment
- 1.6 Nuclear substances and radiation devices
- 2.0 Safety and control areas
- Series 2.1 Management system
- 2.2 Human performance management
- 2.3 Operating performance
- 2.4 Safety analysis
- 2.5 Physical design
- 2.6 Fitness for service
- 2.7 Radiation protection
- 2.8 Conventional health and safety
- 2.9 Environmental protection
- 2.10 Emergency management and fire protection
- 2.11 Waste management
- 2.12 Security
- 2.13 Safeguards and non-proliferation
- 2.14 Packaging and transport
- 3.0 Other regulatory areas
- Series 3.1 Reporting requirements
- 3.2 Public and Aboriginal engagement
- 3.3 Financial guarantees
- 3.4 Commission proceedings
- 3.5 CNSC processes and practices
- 3.6 Glossary of CNSC terminology
Note: The regulatory document series may be adjusted periodically by the CNSC. Each regulatory document series listed above may contain multiple regulatory documents. For the latest list of regulatory documents, visit the CNSC's website.